How to Perform a Safe Cholecystectomy

Safe Cholecystectomy
Achieving the Critical View of Safety is essential for preventing bile duct injury during cholecystectomy. This technique is based on three fundamental requirements: first, the hepatocystic triangle must be completely cleared of all fat and fibrous tissue; second, the lower one-third of the gallbladder must be dissected off the cystic plate to ensure clear separation; and third, only two structures—the cystic duct and cystic artery—should be seen entering the gallbladder.
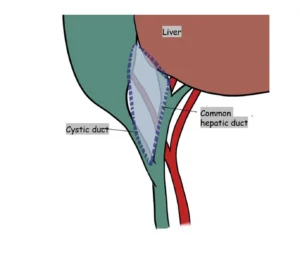
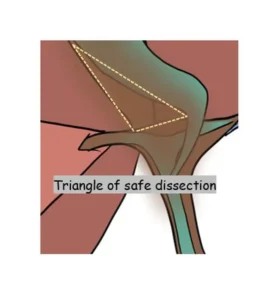
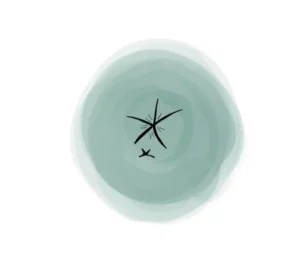
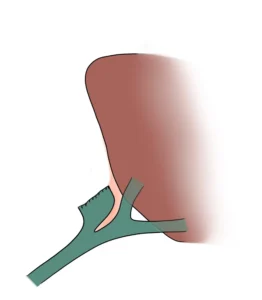
The hepatocystic triangle, the primary target for safe dissection, is bordered medially by the common hepatic duct, laterally by the cystic duct, and superiorly by the undersurface of the liver. Understanding this anatomy, including its potential variations, is crucial for performing a safe and effective cholecystectomy.
Mechanism of Classic Injury
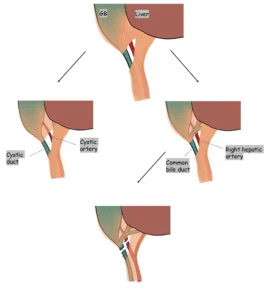
After fully clearing the hepatocystic triangle, the surgeon carefully identifies the two true structures entering the gallbladder—the cystic duct and the cystic artery. Confirming these structures with unobstructed visualization is essential to ensure accurate anatomy, prevent misidentification, and maintain the principles of safe cholecystectomy.
Importance of The Second and Third Criteria of CVS
The risk of injury can be minimized by confirming that only two structures—the cystic duct and cystic artery—are seen entering or leaving the gallbladder, ensuring correct anatomical identification before any division is performed.
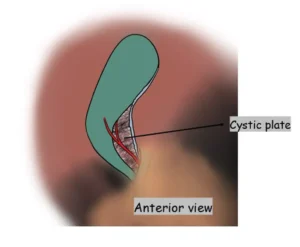
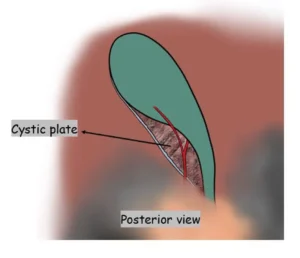
The lower one-third of the cystic plate should be fully exposed on both the anterior and posterior surfaces before any structure is clipped or divided. This ensures clear visualization of the true anatomy and supports safe execution of the Critical View of Safety.
The Cystic Duct
The dissection and ligation of the cystic duct should take place near its junction with the gallbladder. The junction with the bile duct should not be dissected to avoid injury to the bile duct.

The cystic duct may join the bile duct in several anatomical patterns:
A. Most commonly (~75%), it enters the bile duct at an angle.
B. In about 20% of cases, it runs parallel to the bile duct for a variable distance before joining it.
C. Rarely (~5%), it joins the bile duct from the left side.
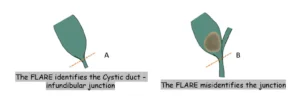
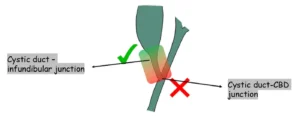
a. In the infundibular approach, surgeons rely on a characteristic “flare” or funnel-shaped appearance to identify the junction between the cystic duct and the gallbladder.
b. However, when the cystic duct is shortened due to a distended gallbladder neck, this method can be misleading and may lead to mistaking the common bile duct for the cystic duct.
The Cystic Artery
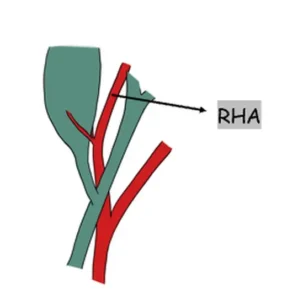
The cystic lymph node is usually located superficially over the cystic artery within the cystic triangle, helping indicate the artery’s position during dissection. When the node cannot be safely separated from the underlying artery, clipping should be performed to the right of the node. This approach reduces the risk of inadvertently injuring the right hepatic artery, enhancing overall surgical safety.

Cystic artery variants
A. Single artery dividing into one superficial and one deep branch near the gallbladder wall- most common (~72%).
b. Multiple arteries in the hepatocystic triangle , due to early branching (~22%).
c. Cystic artery may be caudal to the cystic duct, especially when arising from an anomalous RHA (~6%).

The right hepatic artery may occasionally follow a tortuous course known as the “caterpillar turn” or "Moynihan’s hump.” In this variation, the artery loops close to or within the hepatocystic triangle, increasing its vulnerability during dissection. Surgeons must recognize this pattern to avoid inadvertent arterial injury when performing a cholecystectomy.
Retraction of Gallbladder

The gallbladder fundus should be retracted upward and toward the patient’s right shoulder to provide optimal exposure.
A. The infundibulum must be pulled downward and laterally to create a right-angle relationship between the cystic duct and the common hepatic duct.
B. Incorrect retraction may align the cystic duct and common bile duct in a straight line, increasing the risk of bile duct injury.
For safe posterior dissection, the infundibulum is retracted medially and upward toward the round ligament.
Landmarks for Dissection
The illustration highlights the alignment of the bile ducts as they enter the liver and their relationship to key anatomical landmarks. This spatial orientation helps surgeons understand safe dissection planes, avoid low or misdirected dissection, and maintain proper awareness of critical structures during cholecystectomy.
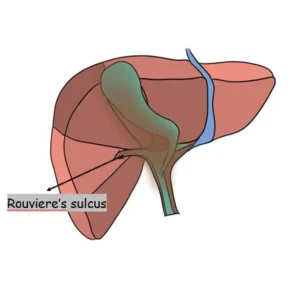
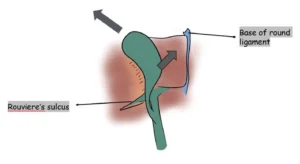
Rouviere’s Sulcus, present in over 75% of patients, is an important anatomical landmark for guiding posterior dissection of the hepatocystic triangle. It contains the right posterior portal pedicle and indicates the level of the hilar plate, helping surgeons avoid dissection that strays too low and reducing the risk of bile duct injury.

Division of the peritoneum located ventral and cephalad to Rouviere’s sulcus is considered safe, as this area lies above the level of the common bile duct. Working within this zone helps maintain proper dissection planes and reduces the risk of inadvertent bile duct injury.
Anteriorly, the base of the quadrate lobe (segment IV) serves as an important landmark, marking the level of the hilar plate. This reference point helps guide safe dissection and maintain correct orientation during cholecystectomy.
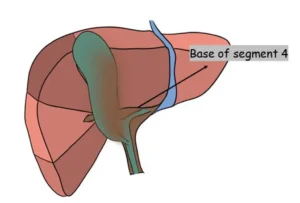
The anterior peritoneum may be safely opened above the plane defined by this line, ensuring dissection remains within a secure zone and reducing the risk of entering structures lying below the level of the hilar plate.

Any dissection done above the level of a line drawn joining the roof of the rouviere’s sulcus and the base of segment 4 (R4U line) is safe.

Planes of Dissection
The subserosal layer of the gallbladder wall is composed of two distinct layers:
• An inner layer, containing rich vasculature and some fibrous tissue
• An outer layer, characterized by abundant fatty tissue
The ideal dissection plane lies between these layers. During dissection, the fatty outer layer (ss-o) is carefully separated from the inner layer (ss-i), which has a smooth, shiny bluish-green appearance.
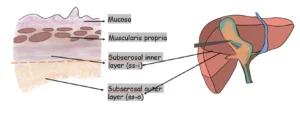
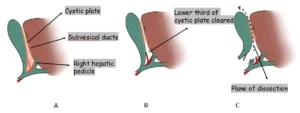
A. The correct dissection plane lies between the gallbladder wall and the cystic plate. Entering deeper than the cystic plate risks bleeding from the liver bed and potential injury to subvesical bile ducts.
B. The lower third of the cystic plate must be fully cleared to achieve the Critical View of Safety.
C. Once the cystic duct and artery are safely divided, the gallbladder is removed by continuing dissection in the plane between the gallbladder wall and the cystic plate.
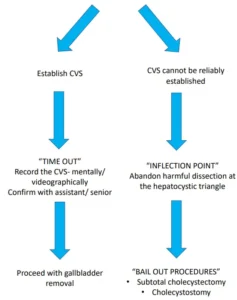
Roadmap for Cholecystectomy
The most crucial step is recognizing when to abandon the standard cholecystectomy technique and transition to a damage-control approach. This decision hinges on identifying situations in which any further dissection within the cystic triangle—even when performed cautiously—poses significant danger and increases the risk of major injury.
Fundus First Technique (Dome Down/ Retrograde)
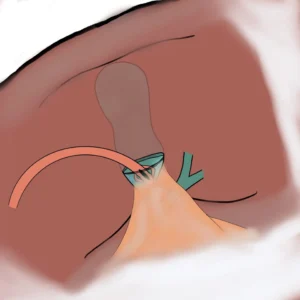
Although the gallbladder is typically separated from the cystic plate in an antegrade manner, it may also be removed retrograde. Because the cystic artery is not ligated before this dissection, increased bleeding from the gallbladder bed is common. A small portion of peritoneum or gallbladder wall is intentionally left at the fundus to facilitate liver retraction.
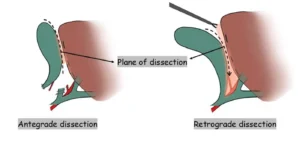
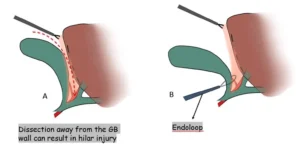
A. Caution must be employed to stay on the wall of the gallbladder. Any deviation from this plain can result in injury to the hilar structures.
B. Endoloops are used for ligation of the cystic duct with the artery en-masse.
Acute Cholecystitis
In acute cholecystitis, the gallbladder—and the cystic plate with it—often becomes shortened, with poorly defined borders. This results in distortion and obscuring of the hepatocystic triangle. The Critical View of Safety is only one element of COSIC (Culture of Safety in Cholecystectomy); having a dependable bailout strategy is equally essential. When the CVS cannot be safely obtained, a subtotal cholecystectomy is the most reliable bailout option.

The anterior gallbladder wall is opened to allow removal of the gallstones. The posterior wall is then dissected and divided from the liver bed, stopping a few centimeters above the R4U line to maintain safety and preserve critical structures.

Fnestrating Subtotal Cholecystectomy
The gallbladder remnant is trimmed to the bare minimum, leaving only a small portion of the wall. The cystic duct may be left open or drained, and the mucosal surface is often cauterized. This technique prioritizes safety by minimizing the risk of bile duct injury in difficult cases.

The cystic duct opening can sometimes be visualized internally using an angled laparoscope, allowing suture ligation from within the remnant infundibulum. However, significant inflammation often makes this approach challenging and technically difficult to perform safely.
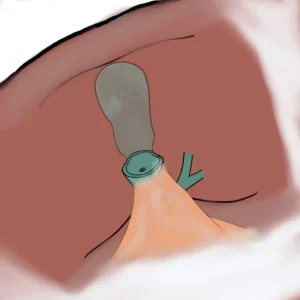
The mucosal surface of the gallbladder remnant is cauterized, and a drain is placed at the infundibulum just above the cystic duct, exiting through the laparoscopic port site. The main drawback of this approach is a higher risk of postoperative bile leakage; however, these fistulas usually resolve spontaneously and this method remains safer than risking a bile duct injury.
Reconstituting Subtotal Cholecystectomy
In the fenestrating type of subtotal cholecystectomy, the gallbladder remnant is trimmed down to the bare minimum. In the reconstituting type, a larger remnant is preserved, which is then closed with sutures to reconstruct a small portion of the gallbladder.
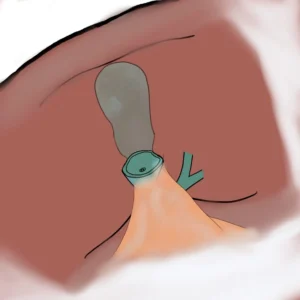
Although postoperative bile leakage is reduced, gallbladder remnants from a subtotal cholecystectomy can become symptomatic years later, potentially leading to recurrent pain, inflammation, or the need for further intervention.
Frequently Asked Questions
Safe cholecystectomy relies on obtaining the Critical View of Safety, clearly identifying the cystic duct and artery before division, and avoiding blind clipping or cutting. Surgeons should use traction techniques to expose Calot’s triangle, recognize anatomic variations, and switch to alternative strategies—subtotal cholecystectomy, fundus-first approach, or conversion to open—whenever dissection becomes unsafe or anatomy remains unclear.
The triangle of safety (Calot’s triangle modern interpretation) is the area bordered by the cystic duct, common hepatic duct, and inferior surface of the liver. Dissection within this zone—after clearing fat and fibrosis—allows visualization of the cystic structures. Achieving the Critical View of Safety within this triangle minimizes the risk of bile duct injury during laparoscopic or open cholecystectomy.
The Safe Cholecystectomy Task Force, formed by the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), develops guidelines to reduce bile duct injuries. It promotes standardized practices such as obtaining the Critical View of Safety, recognizing hazardous anatomy, adopting bailout procedures, and enhancing surgeon education. Its recommendations help unify global standards for performing safer cholecystectomies across varying clinical environments.
