The liver is a vital organ involved in digestion, detoxification, and metabolism. Damage to liver cells can occur due to various underlying conditions. Understanding the different types of liver disease, cause of liver disease, can liver disease be cured is essential for early detection, proper treatment, and prevention of complications such as liver failure or cancer.
What is Liver Disease?
Liver disease refers to any condition that negatively affects the structure or function of the liver. As the body’s largest internal organ, the liver performs vital roles such as detoxifying the blood, producing bile for digestion, and regulating metabolism. When the liver becomes damaged due to infection, inflammation, injury, or chronic habits like alcohol consumption, it can lead to a range of disorders collectively referred to as liver disease.
How Common is Liver Disease?
Liver disease affects over 1.5 billion people worldwide, making it one of the most common health conditions globally. From fatty liver and hepatitis to cirrhosis and liver cancer, these conditions are increasing rapidly due to lifestyle issues, alcohol use, and viral infections.
- Non-Alcoholic Fatty Liver Disease (NAFLD) now affects 1 in 4 people globally. Poor diet, lack of exercise, and obesity are the biggest causes.
- India is heavily affected, with liver disorders among the top 10 causes of death. Alcohol-related liver disease and viral hepatitis are major contributors.
Early Signs and Symptoms of Liver Disease
Liver disease often develops silently in its early stages. Because the liver can function even when partially damaged, symptoms may not appear until the condition has advanced. However, there are several warning signs that may indicate the onset of liver problems. Recognizing these early can help in identifying different types of liver disease before they cause serious harm.
- Fatigue and Weakness: Constant tiredness or lack of energy is often one of the earliest signs. It occurs because the liver can no longer effectively remove toxins or regulate nutrients.
- Loss of Appetite and Weight Loss: A sudden decrease in hunger, along with unexplained weight loss, may signal liver dysfunction. It’s especially concerning when accompanied by nausea or bloating.
- Yellowing of Skin or Eyes (Jaundice): When the liver fails to process bilirubin, it builds up and causes a yellowish tint. This is a classic and visible sign of liver trouble.
What are The Causes of Liver Disease?
Liver disease results from various factors that damage the liver over time. These causes may be genetic, infectious, lifestyle-related, or even autoimmune in nature. Understanding the causes of liver disease is essential for prevention, early diagnosis, and effective treatment.
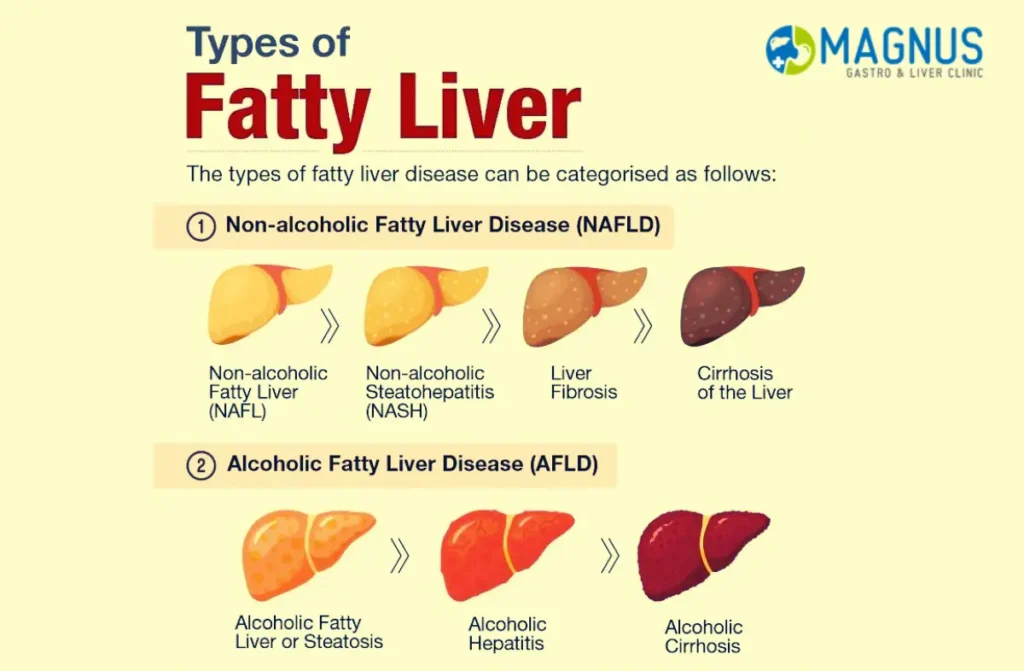
- Non-Alcoholic Fatty Liver Disease (NAFLD): Excess fat buildup in the liver, not caused by alcohol, is often linked to obesity, diabetes, and metabolic syndrome.
- Chronic Alcohol Consumption: Drinking alcohol regularly over a long period can damage liver cells, leading to fatty liver, alcoholic hepatitis, and eventually cirrhosis.
- Viral Infections (Hepatitis B, C, and D): Viral hepatitis is a leading cause of liver inflammation and long-term damage. Hepatitis A, B, and C, if untreated, can lead to liver cirrhosis or liver cancer.
Treatments
Liver disease treatment varies depending on the cause, stage, and overall health of the individual. Some cases respond well to lifestyle changes, while others require long-term medication or even surgery. Many people ask what is the best medicine for liver disease, but effective treatment usually combines medication, monitoring, and lifestyle adjustments tailored to the specific condition.
- Lifestyle Modification: For early-stage non-alcoholic fatty liver disease (NAFLD) and mild alcoholic liver disease, lifestyle changes are the first line of treatment. These include weight loss, a liver-friendly diet, regular physical activity, and quitting alcohol.
- Antiviral Medications: Chronic hepatitis B and C are treated with antiviral drugs that suppress or eliminate the virus. Hepatitis C is often curable with direct-acting antivirals (DAAs), while hepatitis B can be controlled with lifelong medications like tenofovir or entecavir.
- Immunosuppressive Therapy: Autoimmune hepatitis requires drugs like corticosteroids and azathioprine to control the immune system’s attack on liver cells.
- Chelation and Specific Therapies: Genetic liver disorders such as Wilson’s disease or hemochromatosis are treated with chelating agents or phlebotomy to remove excess metals like copper or iron.
- Supportive Treatments for Cirrhosis: In advanced liver disease, treatment focuses on managing symptoms and preventing further damage. This includes diuretics for fluid retention, beta-blockers to lower portal hypertension, and lactulose for encephalopathy.
- Liver Transplant: For end-stage liver disease or liver cancer, transplant surgery may be the only effective option. A healthy donor liver replaces the damaged one.
Diagnosis and Tests
Diagnosing liver disease accurately requires a combination of medical history, physical examination, blood tests, and imaging. Early detection plays a critical role in preventing severe complications and guiding proper treatment.
1. Physical Examination and History
- A doctor first evaluates symptoms such as fatigue, jaundice, swelling, or pain in the upper abdomen.
- They also assess lifestyle factors like alcohol use, diet, medication history, and family conditions related to liver health.
2. Liver Function Tests (LFTs)
- These are blood tests that measure enzymes and proteins like ALT, AST, ALP, bilirubin, and albumin.
- Abnormal results suggest inflammation, damage, or poor liver performance.
3. Imaging Tests
- Ultrasound: The most common test to detect fatty liver, cysts, or tumors.
- CT Scan or MRI: Used to examine the liver in greater detail, especially for cancer or structural damage.
- FibroScan (Transient Elastography): A specialized ultrasound to measure liver stiffness and assess liver fibrosis or cirrhosis.
4. Viral and Autoimmune Testing
- Blood tests can detect hepatitis A, B, and C, and autoimmune markers to identify the exact cause of inflammation.
- Helps guide treatment, especially in chronic viral hepatitis or autoimmune hepatitis.
5. Liver Biopsy
- A small sample of liver tissue is taken with a needle for microscopic examination.
- It confirms diagnosis, measures disease severity, and helps distinguish between different liver conditions.
6. Genetic and Metabolic Tests
- These tests identify inherited liver diseases like Wilson’s disease or hemochromatosis.
- Useful when liver disease runs in families or when common causes are ruled out.
Prevention and Risk Factors
Liver disease can be significantly reduced or even avoided by managing lifestyle choices and understanding key risk factors. While many wonder what is the best medicine for liver disease, the truth is that in most early-stage cases, prevention is far more effective than any treatment. A healthy routine, regular screenings, and avoiding harmful substances are essential steps in protecting liver health.
1. Poor Diet and Obesity
- Risk: A high intake of sugar, processed food, and saturated fats leads to fat accumulation in liver cells. This is a primary cause of non-alcoholic fatty liver disease (NAFLD), especially in people with sedentary lifestyles.
- Prevention: Choose a balanced diet with fruits, vegetables, whole grains, and healthy fats. Engage in regular physical activity and maintain a healthy weight.
2. Excessive Alcohol Consumption
- Risk: Prolonged and heavy drinking causes inflammation and scarring in the liver. Alcoholic liver disease is one of the most common and preventable forms of liver damage.
- Prevention: Limit alcohol consumption or avoid it entirely. If liver function is already compromised, complete abstinence is crucial.
3. Viral Hepatitis (Hepatitis B and C)
- Risk: Chronic hepatitis infections silently damage liver tissue over time and can lead to cirrhosis or liver cancer if untreated.
- Prevention: Get vaccinated against hepatitis B. Avoid sharing needles, and use protection during sexual activity. Early testing and antiviral medications help control viral load.
4. Overuse of Medications and Exposure to Toxins
- Risk: Long-term or high-dose use of over-the-counter painkillers, herbal supplements, and exposure to industrial toxins can harm liver cells and impair function.
- Prevention: Always follow medical guidance when using medications. Avoid self-medicating and be cautious with unregulated supplements or toxic environments.
5. High Blood Sugar and Cholesterol
- Risk: People with diabetes or elevated cholesterol are at increased risk of fatty liver disease due to fat buildup and inflammation.
- Prevention: Keep blood sugar and lipid levels within normal range through diet, regular exercise, and medication when needed.
6. Genetic and Autoimmune Conditions
- Risk: Some liver diseases are inherited or immune-related, such as hemochromatosis, Wilson’s disease, or autoimmune hepatitis. These may go unnoticed until significant damage occurs.
- Prevention: If there’s a family history of liver disease, consider regular screening. Early diagnosis allows timely treatment and prevents complications.
Conclusion
To sum up, if you are experiencing any of the symptoms or different types of liver disease as mentioned above, it is important to consult a healthcare professional as soon as possible because early diagnosis and treatment can prevent serious complications and improve long-term outcomes.
Read also What is a Liver Function Test?




