Liver failure is a serious medical condition where the liver loses its ability to function properly, either due to a sudden injury or long-term damage. As the central organ responsible for filtering toxins, producing vital proteins, and supporting digestion, any disruption to its processes can be life-threatening. Identifying the signs of liver failure early is critical, as timely intervention can prevent further deterioration. These signs often begin subtly but may quickly progress, signaling the liver’s declining capacity. Understanding the causes and symptoms can help individuals take proactive steps toward liver health and avoid complications.
What is Liver Failure?
Liver failure happens when the liver can no longer carry out its essential functions, developing either slowly over time (chronic) or rapidly (acute). It disrupts essential processes such as detoxifying the blood, producing proteins for clotting, and regulating metabolism, posing a serious risk to overall health and survival.
- Early indicators of liver failure can appear gradually, often presenting as ongoing tiredness, frequent nausea, and reduced interest in eating. As liver damage progresses, jaundice (yellowing of the skin and eyes), swelling in the abdomen, confusion, and a tendency to bleed or bruise easily can become more prominent.
- Signs of liver failure from alcohol often develop after prolonged heavy drinking and include abdominal pain, especially in the upper right side, jaundice, and frequent episodes of vomiting. A common early warning sign is alcoholic hepatitis, where the liver becomes inflamed and tender, potentially progressing to cirrhosis if alcohol use continues.
- Signs of acute liver failure typically appear rapidly, sometimes within days, even in individuals without pre-existing liver disease. These can include sudden confusion or disorientation (hepatic encephalopathy), bleeding disorders, and severe fatigue, often requiring urgent hospitalization and possible liver transplantation.
- Signs of imminent death from liver failure include deepening jaundice, unresponsiveness, severe fluid accumulation in the abdomen, and a marked decline in kidney and brain function. Patients may enter a coma-like state, signaling the final stages of multi-organ failure due to the liver’s inability to support critical life functions.
- Liver biopsy is often a key diagnostic tool in evaluating the extent and nature of liver damage. By examining a small tissue sample under a microscope, doctors can determine the cause of liver dysfunction, assess disease severity, and guide appropriate treatment decisions.
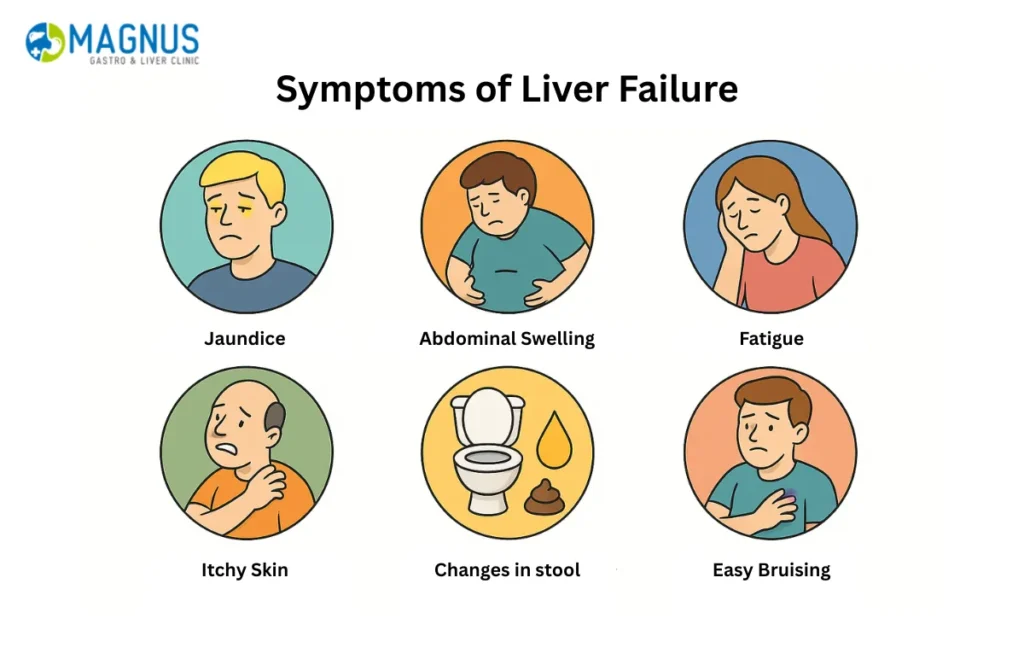
Signs of Liver Failure
Liver failure occurs when the liver loses its ability to perform essential functions such as filtering toxins, producing bile, and managing proteins vital for blood clotting. Recognizing the signs of liver failure early can be life-saving, as timely medical attention can help prevent irreversible damage. Below are some of the most important indicators to watch for:
- Jaundice (Yellowing of Skin and Eyes): One of the first and most visible signs of liver failure is jaundice. It happens when bilirubin builds up in the blood due to the liver’s inability to process it, causing a yellowish tint to the skin and eyes.
- Swelling in Abdomen and Legs: Fluid retention in the abdomen (ascites) and lower limbs (edema) can indicate declining liver function. This is often due to increased pressure in the liver’s veins and decreased production of albumin, a protein responsible for maintaining fluid balance.
- Fatigue and Weakness: The accumulation of toxins in the bloodstream can lead to extreme tiredness, confusion, and poor concentration. Persistent fatigue is one of the first signs of a bad liver, showing that the liver is struggling to filter harmful substances efficiently.
- Bruising and Bleeding Easily: Since the liver produces proteins necessary for blood clotting, failure in this function can lead to unexplained bruises or prolonged bleeding from minor injuries.
- Loss of Appetite and Weight Loss: A noticeable decrease in appetite and unintended weight loss often occur as the body struggles with metabolic imbalance. These may also accompany nausea, vomiting, or bloating after meals.
- Mental Confusion (Hepatic Encephalopathy): When the liver fails to remove toxins from the blood, they accumulate in the brain, causing confusion, forgetfulness, and even coma in severe cases. This is a critical warning among signs of acute liver failure.
- Dark Urine and Pale Stool: Dark-colored urine and clay-like stool indicate bile flow obstruction. It’s another one of the first signs of a bad liver suggesting compromised bile processing.
- Severe Itching (Pruritus): The buildup of bile salts beneath the skin leads to persistent itching. This symptom worsens as liver function deteriorates and can significantly affect sleep and daily comfort.
- Abdominal Pain and Discomfort: Dull or sharp pain in the upper right abdomen could signal liver inflammation or swelling. This pain may worsen after meals or alcohol consumption.
Symptoms of Liver Failure
The signs of liver failure from alcohol and other causes often progress from mild to severe. As the condition advances, the body exhibits systemic symptoms that demand urgent medical attention.
- Nausea and Vomiting: Continuous nausea or vomiting suggests that the liver is unable to handle toxins effectively. This symptom is particularly prominent in individuals with signs of liver failure from alcohol abuse.
- Confusion and Personality Changes: Cognitive decline, forgetfulness, and mood swings occur as toxins reach the brain. These are advanced signs of acute liver failure and may rapidly worsen without treatment.
- Bleeding Gums and Nosebleeds: Reduced clotting factor production increases the risk of spontaneous bleeding, even from small cuts or dental cleaning.
- Severe Swelling and Fluid Accumulation: The presence of large volumes of fluid in the abdomen signifies advanced liver disease, which can cause shortness of breath and intense discomfort.
- Coma or Unresponsiveness: As liver failure progresses toward its final stages, the patient may become unresponsive. These are signs of imminent death from liver failure and require palliative management to ease discomfort.
- Multiple Organ Dysfunction: In end-stage cases, other organs like the kidneys or brain begin to fail. These are recognized as Signs of death from liver failure, where the body’s systems can no longer sustain essential functions.
- Drop in Blood Pressure and Temperature: During the final stages, the patient may experience low blood pressure, cool skin, and shallow breathing — further Signs of death from liver failure, marking the body’s gradual shutdown.
Understanding these warning signals allows early detection and timely intervention, potentially improving survival and quality of life.
What are the Stages of Liver Failure?
Liver failure develops in progressive stages, each marked by worsening liver dysfunction and increasingly severe symptoms. Understanding these stages helps in early identification, timely intervention, and management of complications related to liver damage.
- Stage 1: Inflammation is the earliest phase, where liver cells become irritated and inflamed due to infections, toxins, or excessive alcohol consumption. At this stage, there may be few noticeable symptoms, but signs of liver failure from alcohol such as fatigue, abdominal discomfort, and nausea can begin to surface.
- Stage 2: Fibrosis occurs when ongoing inflammation leads to the development of scar tissue in the liver. While the liver still functions relatively well, subtle signs like mild jaundice, digestive issues, and swelling may appear, and liver damage becomes more difficult to reverse without intervention.
- Stage 3: Cirrhosis is characterized by extensive scarring that severely limits liver function. Common signs of liver failure, including fluid buildup in the abdomen (ascites), leg swelling, and easy bruising, become more visible, especially in individuals with chronic alcohol use or hepatitis.
- Stage 4: End-stage liver disease (ESLD) represents the final phase, where the liver can no longer perform its vital functions. Signs of acute liver failure and hepatic encephalopathy such as confusion, drowsiness, and internal bleeding are often present, and liver transplantation may be the only life-saving option.
- Stage 5: Multi-organ failure and death can follow if liver failure remains untreated, especially in acute cases. Signs of imminent death from liver failure include deep jaundice, complete loss of consciousness, kidney failure, and respiratory distress, indicating systemic collapse and a critical medical emergency.
What Causes Liver Failure?
Liver failure results from prolonged damage or sudden injury to liver cells, impairing the organ’s ability to function. Understanding the root causes is critical for prevention, early recognition of the signs of liver failure, and timely medical management.
- Chronic alcohol abuse: One of the most common causes, excessive and long-term alcohol consumption leads to liver inflammation, fatty liver, alcoholic hepatitis, and eventually cirrhosis. The signs of liver failure from alcohol often begin subtly but can progress to severe complications if alcohol intake continues.
- Viral hepatitis (especially Hepatitis B and C): These infections cause gradual liver damage over years, leading to chronic inflammation and fibrosis. Without treatment, they can progress to cirrhosis or hepatocellular carcinoma, both of which significantly increase the risk of liver failure.
- Non-alcoholic fatty liver disease (NAFLD): Closely linked to obesity, diabetes, and metabolic syndrome, this condition begins with fat accumulation in the liver. If it progresses to non-alcoholic steatohepatitis (NASH), it may lead to cirrhosis and liver failure, often showing overlapping symptoms with early signs of liver failure.
- Drug-induced liver injury: Medications such as acetaminophen (paracetamol) in high doses are a leading cause of signs of acute liver failure. Herbal supplements, antibiotics, and some anesthetics can also cause sudden, severe liver damage in susceptible individuals.
- Autoimmune hepatitis and genetic disorders: Autoimmune conditions, where the body attacks liver cells, and inherited diseases like Wilson’s disease or hemochromatosis can gradually destroy liver tissue. These causes often present in younger individuals and may lead to early liver dysfunction.
- Toxins and poisonous substances: Exposure to industrial chemicals, poisonous mushrooms (e.g., Amanita phalloides), or contaminated food can cause rapid and irreversible liver cell death. These often lead to signs of acute liver failure that require immediate medical care.
- Cancer-related liver failure: Advanced stages of liver cancer or metastatic cancers such as pancreatic cancer can directly compromise liver function. When cancerous growths block bile ducts or infiltrate liver tissue, they can cause the liver to fail and may result in symptoms indicating approaching death from liver failure.
What are the Complications or Effects of Liver Failure?
Liver failure can lead to widespread and severe complications affecting multiple organ systems. These complications often develop rapidly in acute cases and progressively in chronic conditions, reflecting the body’s inability to compensate for lost liver function.
- Hepatic encephalopathy: This occurs when toxins like ammonia build up in the bloodstream and reach the brain, causing confusion, memory loss, and personality changes. In advanced stages, it can progress to coma, especially in those with signs of acute liver failure.
- Ascites and spontaneous bacterial peritonitis (SBP): Liver failure causes fluid buildup in the abdomen, increasing the risk of infection within the peritoneal cavity. SBP presents with fever, abdominal pain, and worsening fatigue, and requires immediate treatment to prevent further deterioration.
- Variceal bleeding: As liver function declines, blood flow through the portal vein becomes obstructed, leading to enlarged veins (varices) in the esophagus and stomach. These varices may rupture, causing life-threatening bleeding, often seen in advanced cases with signs of liver failure from alcohol.
- Coagulopathy and bleeding disorders: The liver produces most clotting factors; when it fails, patients experience excessive bleeding, even from minor injuries. Nosebleeds, gum bleeding, and prolonged clotting times are common indicators.
- Low blood sugar and metabolic imbalances: Since the liver controls glucose regulation, its dysfunction particularly in sudden cases can lead to critically reduced blood sugar levels. Electrolyte imbalances, such as low sodium or potassium, can further complicate the clinical picture and worsen the patient’s prognosis.
- How to keep your liver healthy: Adopting a liver-friendly lifestyle can reduce the risk of liver failure. This includes limiting alcohol intake, maintaining a healthy weight, avoiding exposure to toxins, getting vaccinated against hepatitis viruses, and following a balanced diet rich in antioxidants and fiber to support liver function.
How is Liver Failure Diagnosed?
Diagnosing liver failure involves a combination of clinical evaluation, laboratory testing, and imaging studies to assess the liver’s structure and function. Early identification of signs of liver failure can help guide treatment and prevent progression to irreversible stages.
- Physical examination and medical history: Doctors assess symptoms such as jaundice, abdominal swelling, mental confusion, and fatigue. A detailed history of alcohol use, medication intake, and prior liver disease is essential to identify risks, especially in patients showing signs of liver failure from alcohol.
- Blood tests (Liver Function Tests – LFTs): These measure enzymes like ALT, AST, ALP, and bilirubin to determine how well the liver is working. Elevated levels suggest inflammation or damage, while changes in albumin and clotting factors point toward impaired synthetic function in advanced liver failure.
- Coagulation profile and ammonia levels: Prothrombin time (PT/INR) helps assess the liver’s ability to produce clotting factors, and prolonged times suggest severe dysfunction. Elevated ammonia levels are often associated with hepatic encephalopathy, one of the key signs of acute liver failure.
- Imaging studies: Ultrasound, CT scan, or MRI can detect structural abnormalities such as cirrhosis, fatty liver, or tumors. These tools help visualize complications contributing to the signs of liver failure and assess for obstruction or vascular changes.
- Liver biopsy: A small tissue sample is examined under a microscope to confirm the diagnosis and determine the extent of liver damage. It is especially useful in evaluating unexplained liver dysfunction or in chronic cases with overlapping signs of liver failure from alcohol and other causes.
- Monitoring mental and renal status: Confusion, disorientation, and changes in consciousness levels are monitored closely as they may signal signs of imminent death from liver failure. Simultaneously, kidney function tests help detect complications like hepatorenal syndrome.
What is the Treatment for Liver Failure?
Managing liver failure is based on the root cause, the extent of liver damage, and whether it is a sudden (acute) or long-term (chronic condition. Prompt intervention can reverse damage in early stages, while advanced cases often require intensive care or liver transplantation, especially in patients showing signs of acute liver failure or signs of imminent death from liver failure.
- Supportive hospital care: In cases of acute liver failure, patients are closely monitored in an intensive care setting. Supportive treatment includes managing fluid balance, electrolytes, and blood sugar levels, while also preventing complications like infections and cerebral edema.
- Medications to treat the cause: Antiviral drugs for hepatitis B, corticosteroids for autoimmune hepatitis, or chelation therapy for Wilson’s disease may be used depending on the specific cause. In cases showing signs of liver failure from alcohol, abstinence combined with nutritional support and medications like corticosteroids or pentoxifylline can improve outcomes.
- Management of complications: Treatment includes diuretics for ascites, lactulose and rifaximin for hepatic encephalopathy, and beta-blockers or band ligation for variceal bleeding. Each therapy targets specific complications that emerge as liver function worsens.
- Plasmapheresis or dialysis: In severe acute liver failure, these therapies may temporarily support the body by removing toxins when the liver is unable to filter them. They serve as bridging treatments until recovery or transplant becomes possible.
- Nutritional support and alcohol cessation: Patients with malnutrition or signs of liver failure from alcohol benefit significantly from dietary modifications and complete avoidance of alcohol. High-protein diets are often restricted in cases of encephalopathy to reduce ammonia production.
- Liver transplantation: This is the only definitive treatment for end-stage liver disease or fulminant hepatic failure. Candidates with signs of imminent death from liver failure are prioritized for transplantation, which can be life-saving if performed in time.
Conclusion
Recognizing the signs of liver failure early is crucial for improving treatment outcomes and preventing irreversible damage. Whether caused by chronic alcohol use, viral infections, metabolic disorders, or acute injuries, liver failure can rapidly escalate without proper care. Timely medical intervention, lifestyle changes, and long-term monitoring are essential to slow progression and manage symptoms. Preventive strategies such as avoiding alcohol, maintaining a healthy weight, managing chronic conditions, and ensuring vaccination against hepatitis viruses can significantly reduce the risk of liver failure. Prioritize liver health through regular checkups and early evaluation of any unusual symptoms.
Read Also: Digestive Disorders in Children




