The gut and brain may seem like distant organs, but they’re deeply intertwined through a complex network of nerves, chemicals, and signals. This relationship, often referred to as the gut and brain connection, plays a crucial role in everything from digestion to mood regulation. The gut, often called the second brain, houses millions of neurons and produces neurotransmitters like serotonin. These signals travel to the brain, influencing emotions, behavior, and even cognitive function. Understanding this connection helps explain why stress affects digestion or why certain foods impact mental clarity. In the sections ahead, we’ll explore how this powerful link shapes both physical and mental health.
How Does the Gut-Brain Connection Work?
The gut and brain connection is a two-way communication system involving the central nervous system, the enteric nervous system, and a vast network of biochemical signals. This connection influences both physical digestion and mental well-being, forming the basis of what scientists call the brain-gut axis.
- Vagus Nerve Communication: The vagus nerve is the primary pathway that links the stomach and brain connection. It transmits information between the brain and gut in real time, helping regulate digestion, inflammation, and even mood by carrying signals such as stress responses and gut discomfort.
- Neurotransmitter Production in the Gut: The gut produces key neurotransmitters like serotonin and dopamine, which are typically associated with mood regulation. In fact, over 90% of the body’s serotonin is found in the digestive tract, making the gut a central player in emotional balance and mental clarity.
- Gut Microbiome’s Role: The trillions of microbes in the gut play a major role in the brain-gut connection anxiety relationship. Certain gut bacteria can influence stress levels and emotional behavior by producing neuroactive compounds, which either calm or stimulate the brain depending on their balance.
- Immune System and Inflammation: The gut houses about 70% of the body’s immune system, and chronic gut inflammation can impact the brain. Ongoing inflammation may contribute to conditions like depression or anxiety, reinforcing the strength of the gut and brain connection.
- Diet’s Influence on the Brain: What we eat directly impacts how our gut communicates with the brain. A gut-brain connection diet, rich in fiber, fermented foods, and omega-3s, supports beneficial bacteria and reduces inflammatory responses that may otherwise disrupt mental function.
Impact of Digestion on Mental Health Conditions
The gut and brain connection plays a pivotal role in shaping emotional and psychological well-being. Disturbances in digestion can send stress signals to the brain, while mental strain can disrupt gut function, creating a continuous feedback loop that affects mental health.
- Anxiety and Digestive Imbalance: A disrupted digestive system can trigger or worsen anxiety, illustrating the strength of the brain-gut connection anxiety link. When gut bacteria are imbalanced, they may produce excess stress-related chemicals, which in turn activate the brain’s anxiety pathways.
- Depression and Serotonin Production: Since most serotonin is produced in the gut, poor digestion or inflammation can significantly reduce its availability. Low serotonin levels are closely associated with depressive symptoms, highlighting how gut dysfunction directly influences mood disorders.
- Stress-Related Gastrointestinal Symptoms: Chronic stress can slow or accelerate digestion, leading to symptoms like bloating, cramps, or constipation. These physical discomforts often intensify emotional distress, reinforcing the stomach and brain connection in conditions like IBS and generalized anxiety disorder.
- Influence of Diet on Mood Disorders: A poor diet high in sugar and processed foods can inflame the gut and disrupt the microbiome, leading to cognitive fog and irritability. Conversely, a well-balanced gut-brain connection diet rich in prebiotics, probiotics, and healthy fats supports mental clarity and emotional resilience.
- Inflammation and Cognitive Decline: Ongoing gut inflammation may release cytokines chemical messengers that influence brain function. Elevated cytokine levels have been linked to memory problems and increased risk of depression, underscoring the long-term mental health impact of poor digestive health.
Gut is Responsible for Your Mood its health directly affects neurotransmitter levels, immune responses, and emotional balance, making it a central factor in both digestion and mental well-being.
How to Improve Gut-Brain Connection?
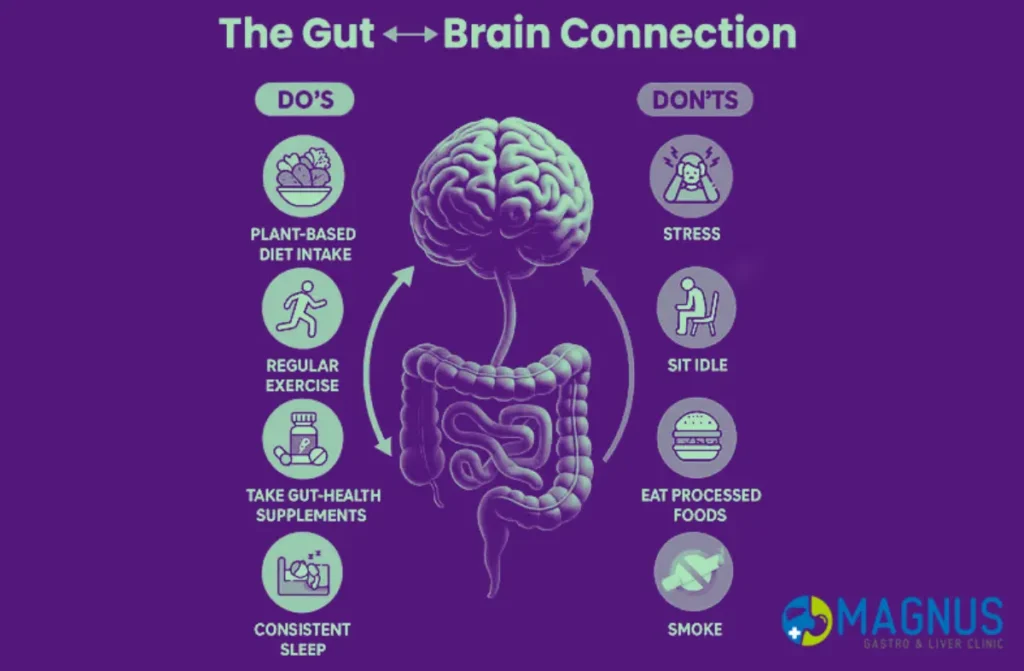
Enhancing the gut and brain connection requires a holistic approach that includes dietary changes, stress management, and healthy lifestyle habits. By supporting both digestive and neurological functions, it’s possible to improve mood, focus, and overall emotional resilience.
- Follow a Gut-Brain Connection Diet: A nutrient-rich diet with high fiber, fermented foods like yogurt and kimchi, and prebiotic-rich vegetables such as leeks and asparagus can strengthen gut flora. These foods support the production of brain-friendly compounds like serotonin, improving emotional stability and the brain-gut connection anxiety response.
- Prioritize Probiotics and Prebiotics: Probiotics add beneficial bacteria to the gut, while prebiotics serve as fuel for these microbes. This combination enhances the stomach and brain connection by promoting a balanced microbiome that communicates more effectively with the brain.
- Practice Stress Reduction Techniques: Chronic stress disrupts gut function and alters microbial diversity. Meditation, deep breathing, yoga, and time in nature can reduce cortisol levels, supporting a calm and balanced gut and brain connection.
- Get Consistent, Quality Sleep: Sleep influences both gut bacteria composition and brain function. Poor sleep increases inflammation and weakens gut barrier function, so 7–9 hours of quality sleep per night is crucial for strengthening the brain-gut connection.
- Engage in Regular Physical Activity: Movement stimulates digestion and increases microbiome diversity. Activities like walking, swimming, or cycling improve gut motility and mood, enhancing the connection between brain and gut through better circulation and hormone regulation.
- Hydrate Properly: Water supports digestion, nutrient absorption, and elimination of toxins. Dehydration can impair both cognitive performance and gut health, disrupting signals within the stomach and brain connection.
- Limit Sugar and Processed Foods: Diets high in sugar and processed ingredients promote inflammation and gut dysbiosis. Cutting back on these foods reduces mood swings, supports beneficial bacteria, and contributes to a more stable gut-brain connection diet.
- Avoid Overuse of Antibiotics: While necessary in certain conditions, frequent antibiotic use can strip the gut of healthy bacteria. Preserving the microbiome helps maintain a strong line of communication between gut and brain, reducing the risk of anxiety and mood disorders.
- Consume Omega-3 Fatty Acids: Found in fatty fish, flaxseeds, and walnuts, omega-3s support brain health and reduce gut inflammation. These essential fats enhance neuronal signaling and microbial balance, reinforcing the gut and brain connection.
- Include Polyphenol-Rich Foods: Berries, green tea, cocoa, and olive oil are high in polyphenols, which support healthy gut bacteria and cognitive function. These antioxidants play a role in reducing anxiety and improving memory through the brain-gut connection anxiety loop.
How do healthcare providers treat disorders of the gut and brain?
Healthcare providers approach disorders of the gut and brain with a comprehensive strategy, recognizing the intricate link known as the brain-gut connection anxiety. This connection highlights how gastrointestinal issues can influence mental health and vice versa, making integrated treatment essential for effective outcomes.
- Medical Evaluation and Diagnostics: Providers begin with a thorough assessment that includes medical history, physical examination, and diagnostic tests such as endoscopy, imaging, or blood work. This helps identify underlying gut disorders like irritable bowel syndrome, inflammatory bowel disease, or dysbiosis, while also evaluating mental health factors linked to the brain-gut connection anxiety.
- Medication Management: Treatment often involves medications tailored to both gastrointestinal and psychological symptoms. Probiotics, antispasmodics, or anti-inflammatory drugs can improve gut function, while anxiolytics, antidepressants, or other neuro-modulators address anxiety and mood disturbances.
- Dietary and Nutritional Therapy: Customized diets, such as low-FODMAP or fiber-rich plans, help reduce gut inflammation and regulate bowel function. Nutritionists also work to correct deficiencies that may impact brain function, supporting overall mental and gastrointestinal well-being.
- Psychological and Behavioral Interventions: Cognitive-behavioral therapy, mindfulness practices, and stress management techniques are commonly employed. These therapies help patients manage anxiety, improve gut motility, and strengthen the brain-gut connection anxiety through behavioral and emotional regulation.
- Integrated and Multidisciplinary Care: Complex cases often require collaboration among gastroenterologists, neurologists, psychiatrists, and dietitians. This approach ensures both the digestive system and mental health are addressed simultaneously, optimizing long-term health outcomes.
- Lifestyle Modifications: Providers encourage regular physical activity, sleep hygiene, and avoidance of alcohol or smoking. These changes help stabilize gut function, reduce systemic inflammation, and positively influence brain chemistry and emotional resilience.
- Emerging Therapies: Novel interventions like gut microbiome modulation, neurofeedback, and personalized psychobiotic treatments are increasingly explored. These strategies aim to restore gut microbial balance while enhancing mental health, further supporting the brain-gut connection anxiety.
Conclusion
The gut and brain connection is a remarkable and complex interplay between your gut health and your internal well-being. Understanding this relationship can empower you to make informed choices about your diet and life to support both your digestive and neurological health. As you’ve learned, the gut-brain axis involves the enteric nervous system, the gut microbiota, inflammation, and the part of diet.
Read Also: Digestive Disorders in Children